UK healthcare industry at the robotics crossroads: Why readiness matters
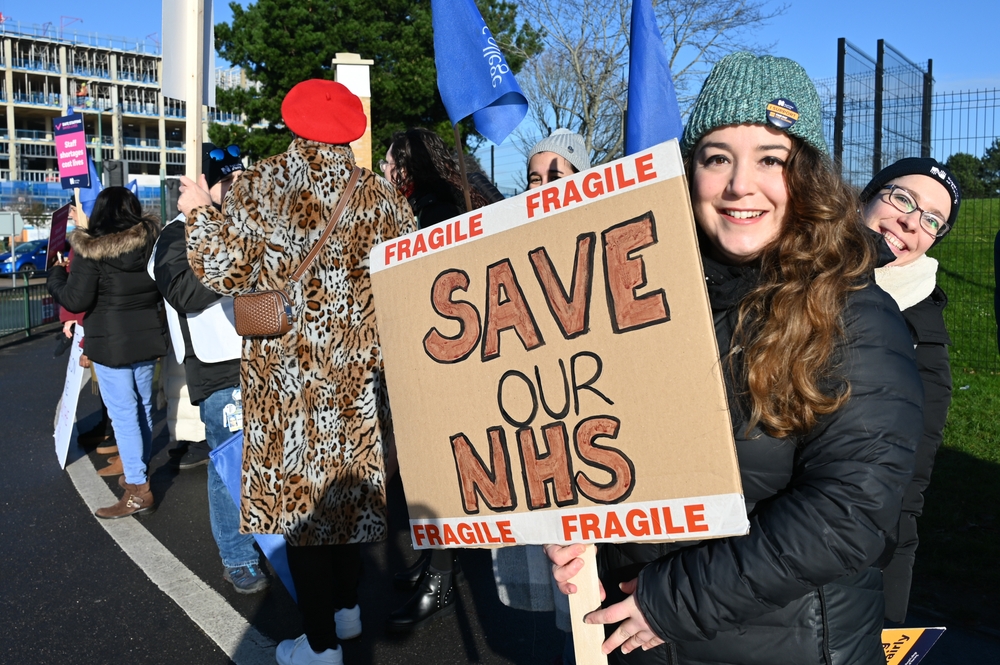
Despite being a global leader in robotics research, the UK lags far behind in real-world adoption – especially in healthcare, where pressures on the NHS are mounting. With billions in potential savings and significant efficiency gains on the table, now is the time to bridge the gap between innovation and implementation, writes Naomi Battison from The National Robotarium.
The UK has always been a little backward when it comes to going forward. We don’t like to rush things. But our adoption of robotics is slow even by our own national standards. While robotic technologies are revolutionising working practices globally, many fear the NHS and healthcare providers here are simply not seeing the potential of robotics to help alleviate the pressures the NHS in particular is facing. Even a modest 0.1 per cent efficiency improvement via robotics could save more than £190 million annually, with greater adoption potentially unlocking billions more in savings and economic value.
The UK’s robotics paradox
Despite being home to world-class academic research in robotics and artificial intelligence, the UK faces a troubling implementation gap. We currently rank just 24th globally in industrial robot density, lagging significantly behind other G7 nations including France and Italy.
However, the democratisation of robotics, driven by the rapid rise of Generative AI, means the technology is increasingly within reach, even for those with challenging budgets constraints.
Challenges and barriers
Health leaders will cite issues such as cost, uncertainty and the challenge of integrating robotics into their processes as barriers to adoption, but this isn’t simply about spending money and purchasing equipment – it requires strategic planning, workforce training, and operational adjustments.
Of course, of critical concern in healthcare is safety, and around a third of UK decision-makers cite safety risks and inadequate policy frameworks surrounding the use of robotics. This may be the reason that promising startups chose to target foreign markets when trialling or launching their tech.
For example, Touchlab has created an electronic skin for robots which enables them to feel almost as humans do. Despite being UK-based, the company had to run its trials in Finland. Similarly, Bioliberty, which is developing a soft robotic glove for stroke rehabilitation, has chosen to launch its tech in the USA.
The readiness gap
But the need far outweighs the risk. With an ageing population and a system already struggling to cope, help must be sought from somewhere.
To address this gap, the National Robotarium in Edinburgh, a world-leading centre in robotics and AI, based at Heriot-Watt University, is launching a series of Robotics Readiness Review Workshops. These sessions provide an unbiased, expert-led assessment of an organisation’s readiness for robotic integration. Participants receive bespoke guidance to help them realistically evaluate their current position, understand available technologies, and plan the steps needed for effective implementation.
The workshops, which are free to attend, are designed to demystify robotics, and create practical roadmaps for adoption that align with each business’s specific needs and capabilities. By addressing common barriers – from technical knowledge gaps to concerns about return on investment – the aim is to accelerate the responsible integration of robotics across the UK.
Proof of concept
There are some good news stories out there.
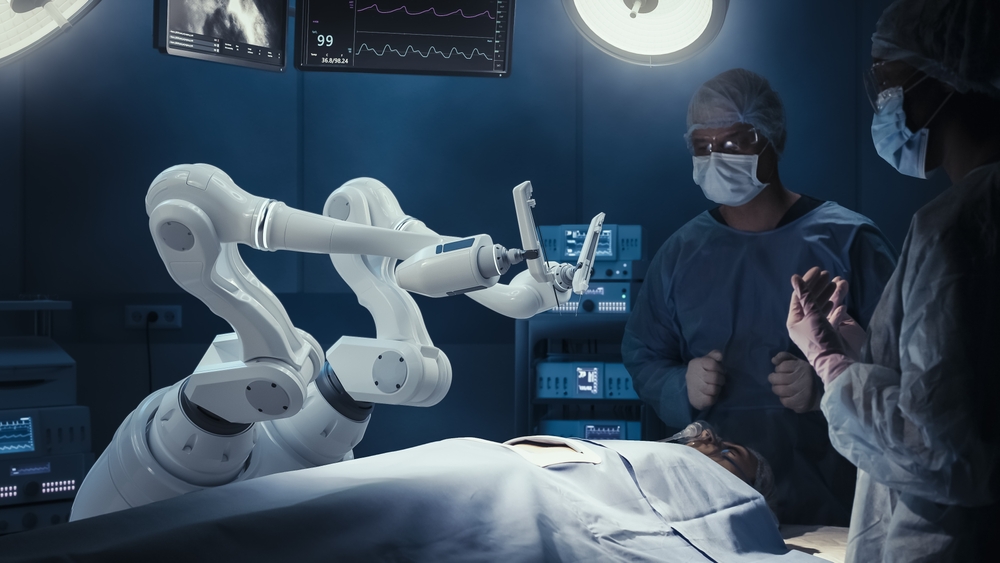
NICE has approved the use of eleven cutting-edge robotic surgery systems for soft tissue and orthopaedic procedures. The technology, which is capable of movements more precise than the human hand, has the potential to transform care for patients being operated on by surgeons in specialist NHS centres.
Indeed, between 2016 and 2023, there were a total of 259,000 robot-assisted procedures carried out in the NHS and private sector. This represents a 524 per cent increase since 2016 (11,180 procedures) to 2023 (69,795 procedures). There is no question that these are encouraging figures.
At Calderdale and Huddersfield NHS Foundation Trust, one robot can perform the work equivalent to 4.5 full-time equivalent staff, with five bots delivering the output of 22.5 staff members. In surgical settings, robotic-assisted surgery (RAS) allows procedures to be completed with fewer team members and enables staff to be redeployed during operations, further improving workflow and productivity.
And just ask the family of four-month-old Mohammed from Manchester for their opinion of robotics in healthcare. Mohammed became the youngest child in the world to successfully have surgery using the Versius Surgical System, which surgeons have called a “game changer” for reconstructive surgery.
If further proof of the benefit of robotics were needed, a study of robotic surgery for radical prostatectomy in the NHS in England found that adopting robotic technology led to a 50 per cent reduction in patient length of stay (LoS), a 49 per cent decrease in post-operative LoS and a 29 per cent improvement in labour productivity among urology surgeons.
The promise of an automated future
The future of the NHS is very much up for debate but a greater willingness to embrace robotic technologies as tools to enhance productivity, efficiency and patient care can surely only be a positive step.
Amazon’s founder Jeff Bezos once said, “When we combine human creativity with robotic precision and endurance, we unlock… possibilities that were previously unimaginable.”
So, the real question is not whether robotics will be transformational, but whether the country will have taken the necessary steps to reap the rewards.
For more information about the National Robotarium’s Robotics Readiness Review Workshops, please contact Naomi at n.battison@hw.ac.uk or visit the National Robotarium website.