A waiting list approach flipped on its head

This is a sponsored article.
Making the Patient Tracking List (PTL) available to general practice in North Central London (NCL) is proving to be an effective approach.
When thinking about how best to address the backlog of patients, it’s natural to only consider the locations where the patients will be treated, but Amy Bowen, director of system improvement for NCL, says her team saw the value of involving primary care in the conversation. “Initially, everyone considered the PTL from secondary care, but we thought ‘let’s flip it on its head’,” she says.
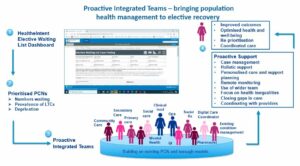
The approach uses funding from the NHS’s elective accelerator sites initiative to form multi-disciplinary Proactive Integrated Teams (PITs) that can access the PTL using the elective recovery dashboard in the Cerner population health platform, HealtheIntent®.
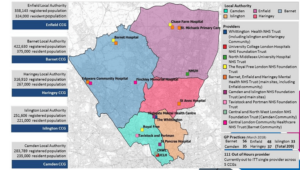
Like a Formula 1 pit crew supports a racing car driver, the objective for the PITs is to use data to optimise and maintain a person’s health while they await treatment. The need is very real across the NCL catchment area, with over 100,000 people having waited over a year for treatment and 300 waiting for more than two years.
The Patient Tracking List is a forward-looking management tool used by the NHS to monitor Referral to Treatment (RTT) and diagnostic waiting times for all patients across England. Even before the pandemic, demand for hospital treatment was outstripping capacity and, with the pressures on delivering care over the past two years, this has led to increased backlogs and longer waits. By April 2022 there were more than two million patients waiting over 18 weeks, with over six million in total waiting for treatment.1
The effort leverages the holistic and long-term nature of the primary care relationship to support people on the PTL. “GPs get the concept easily and they welcomed the fact we were making bandwidth for this,” Bowen says. “This stuff floats my boat because it’s giving people a data-driven, health-inequalities-focused rationale for working together.”
The elective recovery dashboard utilises integrated data from across the system – including primary care – to provide a rich system-to-person view of the elective waiting list. This assists primary care and community teams to prioritise cohorts and more effectively manage patients on the waiting list.
The idea was conceptualised by Katie Coleman, clinical lead for primary care, who says that delivering person-centred and coordinated care is the aspiration of everything she does as a GP.
For Coleman, the PITs are primarily aimed at improving the health of individuals on the waiting list so they can “wait well” and be ready for the procedure when their turn comes up.
“If we can get upstream with their care and identify the things that might prevent them from actually having their surgery, we could then potentially ensure that when they do hit the top of the waiting list that they are in the best space possible,” Coleman says.
The second key element is looking at the wider determinants of health and how a person’s condition impacts their day-to-day life – for example, a person waiting for a hip replacement who is unable to work due to pain.
“If we identify those critical cases that if they don’t have their procedure, they might be at risk of spiralling down that social ladder, we would look to try and help to escalate them and to reprioritise their position in the waiting list,” says Coleman.
The approach is expected to lead to a number of benefits – not only improved health outcomes for the population, but also cost savings for the NHS.
“If you can maximise people’s wellbeing in advance of their procedure, then we know from the research that they have a shorter inpatient stay,” Coleman says. “They have a shorter rehabilitation period, so they’re able to get back up and doing what they need to do quicker.”
Enabling people to get back to work sooner reduces the need for social care and sick leave, and can lead to increased productivity in the workforce.
“Also if we support people to lose weight, bring their blood pressure under control, support them to achieve improved diet, sugar control if they’re diabetic, and so on, all of this over time will also help to drive down the risk of complications,” says Coleman.
“And that obviously has cost savings for the inpatient stay, but also cost savings potentially for the system as a whole.”
NCL’s five boroughs have identified priority cohorts and are working to improve the experience for both patients and care professionals. For example, Haringey is stratifying patients with a diagnosis of severe mental illness combined with two or more long-term conditions.
Jalak Shukla, clinical pharmacist and director of operations for the Haringey GP Federation, says the rationale for this was to provide additional support to patients who are less likely to attend for their procedure when they get to the top of the list.
“It’s a proactive approach, but we’re managing a caseload of patients identified for surgery, making sure they make it, looking after them after the surgery in the communications that they should be receiving, plugging them into the right services, and then putting them back into the care of general practice,” Shukla says.
“All of it’s proactive, all of it’s taken care of and then they can go back to business as usual, accessing the system when they need it.”
An additional benefit of the PITs is the relationship building between primary and secondary care, especially given the fact that post-COVID recovery work is a high priority across the system.
“We know secondary care can’t do it on its own,” Shukla says. “Looking at that list jointly is showing how the system is going to work better together, with primary care picking up what it can to ensure that patients are optimised in the interim.”
The proactive population health management enabled by HealtheIntent is encouraging clinicians to think differently about caseload management.
“We can actually do a one-size-fits-all review for patients and that’s only possible because we’ve got this shared platform,” Shukla says. “The filtering of which long-term conditions they have, their clinical context, their background, their age, the number of contacts that they might have had with the system – all of that data allows you to get a high-level view of what’s going on in your own PCN [primary care network].”
Moving forward, Shukla expects this type of approach to be adopted beyond elective recovery, particularly because of the holistic nature of the approach.
“I think it can make a patient’s journey a lot less fragmented,” she says. “Let’s deal with the long-term condition issues. Let’s deal with the social care issues. Let’s sort out the issues they have with referrals with secondary care. And let’s do it all at once.”
As systems continue to explore ways to meet the demand of the backlog of patients awaiting elective treatment, innovators across the country are using data to help prioritise, optimise and reduce redundancy.
To learn more about how Cerner solutions can support your organisation please visit their population health management solution page.
