Prioritise nutrition and hydration to boost broader health outcomes, says new report

New report from PPP finds that efforts to implement a multidisciplinary approach to nutrition and hydration are needed to help address the dysphagia burden across the NHS.
A new report from Public Policy Projects (PPP) finds that with the UK becoming a ‘super-aged’ society, declining nutritional and hydrational status among elderly and frail populations will place increasing strain on health and care services.
The report, Prioritising nutrition, hydration and dysphagia in an integrated care context, states that while considerable work and investment has been allocated to reduce the incidence of obesity and the diet-related diabetes, malnutrition and hydration are not given the same focus, despite their significant impact on health outcomes and its role in the management of other conditions.
The report is the culmination of two roundtables held by PPP in 2023, which convened stakeholders to discuss how ICSs embed nutritional and hydrational health into integrated care strategies. The discussions focused on specific elements of the debate, including improving the management of dysphagia and care provided for frail populations in different care settings. Attendees included NHS England clinical leadership, allied health professionals (AHPs), including speech and language therapists (SLTs), social care providers, primary care representation nurses and other key health and care stakeholders.
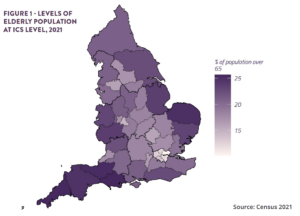
According to the report, recent reforms to the health and care sector (most notably, the introduction of ICSs) present new opportunities to develop comprehensive approaches to nutrition and hydration, in a way that improves holistic patient care and saves valuable resource for the NHS.
However, among its recommendations, the report calls on the Department of Health and Social Care to launch a national review into food and drink provided across the care sector, to help improve the nutritional and hydrational status of frail citizens in social care. This review should follow the structure and ethos of the NHS Hospital Food programme, the report argues.
It adds that addressing dysphagia should be central to broader NHS goals of enhancing the quality of life for the elderly population, and that by prioritising the management and screening of dysphagia, the NHS could prevent avoidable hospital admissions and promote more efficient use of resources across the health and care sector.
To address the complex and multifaceted challenge of dysphagia, with various medical, neurological, and anatomical elements potentially contributing, will require systems to adopt a multidisciplinary approach, says the report. This will necessitate close collaboration between diverse teams of healthcare professionals, each with specialised expertise.
It finds that a multidisciplinary approach that includes speech and language therapists, dietitians, and physicians, is essential for managing dysphagia and addressing the complex healthcare needs of the elderly in a holistic fashion. To help enable this multidisciplinary approach, the report argues that the model of speech and language therapy sitting in community settings should be scaled nationwide, and adopted across ICSs within integrated care strategies. These strategies should also closely involve the voluntary sector.
The report also recommends an expansion of the speech and language therapy workforce, with ring-fenced funding for broader allied health professionals – in line with ambitions set out in the NHS Workforce Plan.
“The nutritional and hydrational needs of our elderly and frail citizens has been neglected for far too long. As the UK moves towards a ‘super-aged’ society, NHS organisations, care providers and integrated care systems must increasingly focus efforts on improving nutritional and hydrational health,” said report author and Group Editor at PPP, David Duffy. “It is vital that resources are orientated to support allied health professionals, particularly speech and language therapists, who play a vital role in maintaining nutritional health for elderly and frail citizens.
“Nobody in the UK should suffer from malnutrition or dehydration in this day and age, especially not our frailest and most vulnerable citizens. We hope that this report will help shine a light, not just on the scale of the problem, but also on achieveable solutions that we believe will help address the terrible burden of dysphagia.”
Recommendations:
- NHS England must prioritise nutrition, hydration and dysphagia as part of its drive to improve system performance and broader health outcomes. Nutrition and hydration management are underdeveloped areas which can help enable success in key national strategies, such as the elective care backlog plan, workforce strategy, the urgent and emergency care plan and the delivery plan for recovering access to primary care.
- Integrated care systems should consider dysphagia and wider nutritional and hydrational health as key parts of preventative health policies that can help future proof local health systems.
- The Department of Health and Social Care (DHSC) should commission a national review into food and drink provided across the care sector. This review should follow the structure and ethos of the NHS Hospital Food programme. The review should be led by a range of stakeholders from within the NHS and social care, as well as representatives from industry and the private sector.
- As the population becomes a ‘super-aged’ society, an integrated strategy is required to manage the health of the elderly and frail population. This should draw upon global and international frameworks provided by the WHO’s ICOPE framework.
- ICSs should ensure that maximising the ‘intrinsic capacity’ of citizens is a key priority within integrated care strategies, to prevent deterioration of health and supplement preventative health policies.
- ICSs should work to prioritise evidence-based nutritional and hydrational approaches within the social care sector, harnessing tools such as nutritional supplements where necessary, to assist those who have difficulty eating, drinking and swallowing.
- The model of speech and language therapy sitting in community settings should be scaled nationwide, and adopted across ICSs within integrated care strategies. These strategies should also closely involve the voluntary sector.
- NHS England should undertake a national dysphagia screening drive to identify individuals as early as possible. Social care staff and AHPs should be trained to conduct dysphagia screenings for all elderly and frail patients in their care, and much like falls, dysphagia should be considered among the primary risks in any risk assessment of elderly and frail patients.
- The speech and language therapy workforce should be expanded with long-term ring-fenced funding for broader allied health professionals.









