10-Year Health Plan must address cancer care failings identified by Darzi

From improving access to care and diagnosis to addressing treatment delays, Lord Darzi’s recent independent investigation highlights the complex web of challenges facing the NHS. In doing so, it also offers a series of starting points for the upcoming 10-Year Health Plan to address.
Cancer remains one of the leading causes of avoidable death in the UK, and despite improvements in survival rates over the past decades, the country still lags behind others in cancer care. Lord Darzi’s recent independent investigation into the NHS in England offers a comprehensive review of the current state of cancer treatment within the NHS and points to several factors that have contributed to its struggles. These include funding constraints, the aftermath of the Covid-19 pandemic, and systemic issues within healthcare management.
Using the failings identified by Lord Darzi as a basis, the upcoming 10-Year Health Plan for the NHS has the chance to radically transform cancer care provision in the NHS.
Rising cancer waits and slowing survival rate improvements
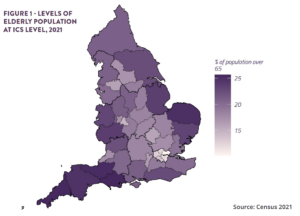
Cancer cases in England have steadily risen, increasing by approximately 1.7 per cent per year from 2001 to 2021. When adjusted for age, the rise is still significant at 0.6 per cent annually. This translates to around 96,000 more cases in 2019 than in 2001. Although survival rates for one-year, five-year, and ten-year intervals have improved, the rate of improvement slowed considerably in the 2010s.
The UK also continues to record substantially higher cancer mortality rates than its peers. International comparisons show the country falling behind not only European neighbours but also the Nordic countries and other English-speaking nations. While survival rates have inched upwards, “no progress whatsoever” was made in early-stage (stage I and II) cancer detection from 2013 to 2021. However, this has recently changed, with detection rates improving from 54 per cent in 2021 to 58 per cent by 2023, partly driven by the success of the targeted lung health check programme. This initiative has helped identify more than 4,000 cases of lung cancer, with over 76 per cent caught at stage I or II, significantly boosting early intervention efforts.
Nonetheless, challenges remain in treatment selection, particularly for brain cancer patients. While genomic testing, critical for tailoring treatments, is now more widespread, only five per cent of eligible brain cancer patients can access whole-genome sequencing. A recent Public Policy Projects (PPP) report has highlighted the inequalities in access to genomic sequencing. Moreover, turnaround times for genomic tests – only 60 per cent of which are processed on time – further hinder timely treatment for many patients.
Access delays and missed treatment targets
One of the key areas within the Darzi investigation is the NHS’ ongoing struggle to meet its cancer treatment targets. The 62-day target from referral to the first treatment has not been met since 2015, and as of May 2024, only 65.8 per cent of patients received treatment within this window. Similarly, over 30 per cent of patients now wait more than 31 days for radical radiotherapy, reflecting growing delays in critical care pathways. Given the importance of timely cancer treatment, the upcoming Plan must consider how to reduce delays in access to treatment.
While the number of cancers diagnosed through emergency presentations has decreased, with the percentage falling from nearly 25 per cent in 2006 to under 20 per cent in 2019, access to primary care services continues to be “uneven”. This affects the timeliness of cancer referrals, especially as the proportion of patients waiting more than a week for a GP appointment rose from 16 per cent in 2021 to 33 per cent per cent by 2024. Darzi notes that declining access to general healthcare services directly reduces the likelihood of timely cancer detection and treatment.
The drivers behind performance issues
Several factors have compounded the challenges facing the NHS’s cancer care system, as identified by Lord Darzi, which the 10-Year Health Plan must seek to address:
- Austerity and capital starvation: Funding restrictions and limited capital investments over the past decade have led to under-resourced healthcare infrastructure, making it difficult to accommodate growing patient demand. The underinvestment in estates and facilities is also preventing the NHS from making full use of diagnostic advancements; in many cases, hospitals may be able to purchase new state-of-the-art diagnostic and imaging equipment, but not have a suitable site in which to use it. PPP has explored this topic in detail in a previous report.
- Covid-19 pandemic: The pandemic severely disrupted healthcare services, creating a backlog of cases and delaying non-Covid-related care, including cancer treatments. Although efforts have been made to prioritise long-waiting patients, the effects of the pandemic still ripple through the healthcare system, contributing to worsened performance.
- Lack of patient voice and staff engagement: The investigation highlights that the perspectives of both patients and healthcare staff have often been overlooked in decision-making processes, resulting in management structures that are out of touch with the realities on the ground. A more engaged and responsive system would likely yield better outcomes. The need for coproduction was reiterated at PPP’s recent Cancer Care Conference, and is increasingly being recognised in Cancer Alliances’ health inequalities strategies.
- Management structures and systems: The report also points to inefficiencies within the NHS’ management structures. These systems are often seen as bureaucratic, which slows down decision-making and the rollout of new treatments. Disparities in the adoption of new systemic anti-cancer therapies highlight these inefficiencies, as some regions wait over a year for access to drugs approved by NICE, while others see the same drugs introduced within a month. This inequality in access to drugs is a key driver of the postcode lottery that is seen in cancer care.
The importance of early diagnosis and screening
A clear priority identified by Lord Darzi is the need for more effective early diagnosis strategies. Cancers detected at stages I and II are much more treatable, and early intervention is strongly associated with better survival outcomes, as well as substantially lower treatment costs. Darzi notes, however, that progress in this area had been stagnant until recent years, with no gains between 2013 and 2021. The improvements seen in early-stage detection from 2021 to 2023 offer hope, but Darzi cautions that further efforts are needed.
The 10-Year Health Plan must also seek to address the UK’s lack of CT and MRI scanners relative to other comparative companies – a major inhibitor of greater diagnostic capacity in the NHS.
Screening participation rates have also declined, with breast and cervical cancer screening coverage falling since 2010. Yet there are signs of promise. For example, the bowel cancer screening programme has been highly successful and provides a model that could be replicated for other types of cancer.
However, hopes for improved early diagnosis cannot rely solely on the establishment of national screening programmes. Poor levels of health literacy, particularly among underserved communities, must also be addressed to ensure that people know which signs and symptoms to be aware of, and to seek treatment if necessary.
More sophisticated treatments but growing delays
The development of more sophisticated treatments is a key area of progress, but the availability of these treatments is often constrained by capacity issues. While the NHS is a world leader in incorporating genomic testing as part of routine cancer care, delays in processing these tests and long waiting times for treatments like radiotherapy undermine their potential impact and can lead to poorer outcomes.
As Darzi points out, “turnaround times are poor… [which] can delay the start of treatment,” especially when coupled with the system’s failure to meet its 62-day target for referral to treatment. In a healthcare system already stretched by rising demand and workforce shortages, delays in treatment can make the difference between life and death for many cancer patients.
Addressing the challenges ahead
Lord Darzi’s investigation underscores the critical need for systemic reforms within the NHS to address the growing cancer burden. From improving access to care and speeding up diagnosis to addressing treatment delays, the report highlights the complex web of challenges facing the NHS. In doing so, it also offers a series of starting points for the upcoming 10-Year Health Plan to address.
While recent advancements in genomic testing and early detection programmes offer hope, the NHS must tackle its systemic inefficiencies, funding shortfalls, and management issues if it is to close the gap with its international counterparts and improve outcomes for cancer patients.
For more information about PPP’s Cancer Care Programme, or to request further discussions, please contact: Rachel Millar, Programme Lead for Cancer Care: rachel.millar@publicpolicyprojects.com
Dr Chris Rice, Director of Partnerships for Cancer Care and Life Sciences: chris.rice@publicpolicyprojects.com