A person-centred, digital first approach to recovery

Ensuring that patient pathways are digitally enabled and person-centred is critical to tackling the elective backlog, writes Patricia Wynn, Director and Sales Leader, International Public Sector Health, Cerner Corporation
NHSE guidance states that “our ambition is to improve core digital and data services in hospitals to ensure we have the basics right.” A leading EPR provider in the UK and globally, Cerner supports systems to reach the minimum digital foundation and strive for HIMSS Stage 7 and beyond.
Cerner work across provider collaboratives to enable shared instances of the EPR. ICS-level collaboration reduces total cost of ownership and enables sharing of resources, such as PMO, training, back office and support. For example, a shared instance of Cerner accelerated provider collaboration across North West London ICS.
Imperial and ChelWest began sharing a domain in 2019 and now London North West and Hillingdon are set to join. According to Kevin Jarrold, ICS data and digital lead, “we have a growing agenda around collaboration across care pathways and the shared domain is absolutely fundamental.”
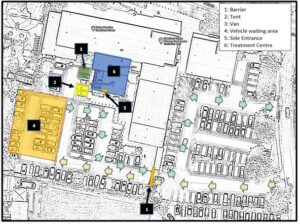
A shared domain has enabled NWL to gain efficiencies and generate much-needed capacity. Leaders can see across the system and transfer patients more effectively from one site to another. Virtual ward capacity is also managed centrally and embedded into the core EPR. Remote patient monitoring is leveraged from a variety of vendors, with all data feeding centrally into virtual wards created within the core EPR, enabling more efficient workflows and the sharing of virtual care staff.
Prioritising care
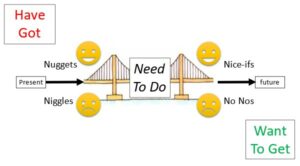
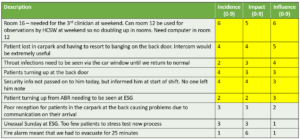
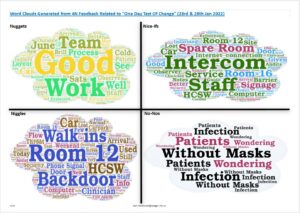
The national guidance outlines care must be prioritised based on clinical urgency, the impact of waiting on individuals and potential inequalities. To achieve this, North Central London (NCL) ICS uses Cerner HealtheIntent®, a data and analytics platform that provides a single longitudinal record for every citizen, comprising data from all health and care organisations across the ICS.
According to Amy Bowen, director of system improvement, “[We built] an elective waiting list dashboard in HealtheIntent. Now we can show GPs for the first time ever what their waiting list looks like. We can cut that data by all the demographic factors, e.g. how many people have long-term conditions and how many? We can look and see by ethnicity, by deprivation – we can combine several factors. And we can actually understand that population at a practice level, at primary care network (PCN) level; by specialty, by borough.”
Transforming care
NHS guidance outlines transformation should focus on flexibility, ease of access and citizen control. Re-envisioning patient pathways – and ensuring they are digitally enabled and person-centred – will be critical. Royal Free London (RFL) has standardised and digitised 40 pathways.
Cerner experts are involved from the beginning of pathway design. Dr John Connolly, CEO of the Royal Free Hospital and group director of clinical pathways shares, “The goal of this ambitious programme is to ensure every patient can get the same high-quality treatment in any of the Trust’s three hospitals… and to create value for the entire healthcare system in the locality – not just our hospitals, but also primary care and public health services in an area that has high levels of deprivation.”
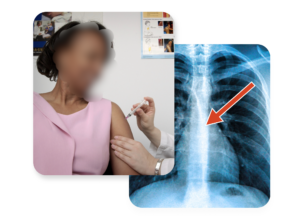
Supporting patients
Ultimately, a person-centred, digital first approach must include the person at the centre. Cerner Patient Portal UK, delivered in collaboration with Induction Healthcare, enables interaction and engagement between caregivers and their populations. A prostate cancer survivor in the Wirral explained, “I cannot emphasise how much the patient portal has improved the quality of my life. Those two weeks of waiting – the stress of revisiting the room where I was given my diagnosis – all that is gone now.”
NHSE’s operating priorities will not be achieved by overworking caregivers and staff, but by enabling them to work smarter and more collaboratively. Contact Cerner Corporation if you share a belief in the power of technology-enabled transformation and want to discuss how Cerner can support your system as in tackling the unprecedented backlog of demand.