First Community Diagnostic Centre Value Partnership with Siemens Healthineers set to improve health outcomes across Teesside

A first-of-its-kind seven-year Value Partnership will see Siemens Healthineers support Tees Valley Community Diagnostic Centre to deliver up to 104,000 checks, scans and tests a year on the high street.
North Tees and Hartlepool NHS Foundation Trust and South Tees Hospitals NHS Foundation Trust have announced the first Community Diagnostic Centre (CDC) Value Partnership to be collaboratively delivered with Siemens Healthineers. The seven-year partnership will set a gold standard for CDCs, placing efficiency, scalability and patient care at its core. Once fully operational, the CDC is set to deliver up to 104,000 potentially lifesaving checks, scans and tests a year.
An impressive fleet of nine imaging systems will be provided, including a variety of CT, MRI, X-ray and ultrasound equipment from Siemens Healthineers. Support includes maintenance of the systems and additional services to bolster prostate cancer pathways and productivity including digital AI, consulting, workforce planning and education. The CDC represents an important investment to improve healthcare outcomes across the region where the proportion of people with major health conditions is at least 10 per cent higher than the national average.
“Integrating advanced imaging systems and AI solutions enables us to provide quicker, more effective diagnostics and treatment while the community setting brings essential services closer to our patients,” said Gail Griffiths, Diagnostic Services Lead for Responsive Care at North Tees and Hartlepool NHS Trust.
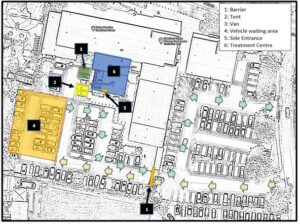
Delivered by the North East and North Cumbria Integrated Care Board, the CDC supports efforts to address health inequalities in the area by ensuring a collaborative, community-based approach, and aligns with government ambitions to move more care away from hospital settings. Access to care outside of a hospital setting means patients can receive more convenient health checks closer to home. The central location in the heart of Stockton town centre alongside a library and leisure centre not only improves access to care, but also encourages a wider transformation of the high street.
The NHS’ 2024/25 priorities and operational planning guidance identifies the opening of new CDCs as a key action for systems, and the upcoming 10-Year Health Plan is expected to reaffirm the value of CDCs for delivering the government’s desire to further shift care in community settings.
Tees Valley CDC will benefit from digital AI solutions as part of the partnership. Utilising AI-Rad Companion from Siemens Healthineers, standardised reporting of the scans will enable quicker, more effective prostate cancer pathways, helping to support both productivity and patient throughput. Support from Siemens Healthineers Consulting includes a tailored transformation programme featuring a project to help increase the daily number of patients receiving MRI scans by up to 40 per cent.1 The partnership will also support upskilling the workforce with tailored training and education opportunities to meet the CDC’s unique requirements.
Among the range of CT, MRI, X-ray and ultrasound equipment from Siemens Healthineers are two SOMATOM X.cite CTs. Both systems are designed with patient experience in mind, equipped with the unique guidance of myExam Companion to automate results, as well as Tin Filter technology to optimise dose efficiency. Tees Valley CDC will also include two MAGNETOM Sola MRI systems, a YSIO X.pree X-ray and two ACUSON Sequoia ultrasound systems from Siemens Healthineers. The wide range of systems will support the delivery of care with the potential for one-stop clinics in the future for diagnostic tests conveniently based in the centre of Stockton.
Kelly Smith, Head of Radiology at South Tees Hospitals NHS Foundation Trust, commented: “In partnership with North Tees and Hartlepool NHS Foundation Trust and Siemens Healthineers we are making a significant step forward in improving healthcare outcomes across the Teesside region. By bringing imaging technology and comprehensive AI solutions to a community setting, we’re not only enhancing diagnostic capabilities but also ensuring more accessible healthcare for our patients.”
“Together with South Tees Hospitals NHS Foundation Trust and Siemens Healthineers we aim to transform healthcare delivery in our region and significantly improve outcomes, added Gail Griffiths.
Ghada Trotabas, Managing Director of Siemens Healthineers Great Britain & Ireland, stated: “This groundbreaking collaboration with North Tees and Hartlepool NHS Foundation Trust and South Tees Hospitals NHS Foundation Trust is the first of its kind for community diagnostics centres. Located in a high street setting, the centre will set a new benchmark for delivering efficient services outside of the hospital environment, bringing care closer to the patients who need it most.
“Our partnership ensures the CDC stays adaptable to the evolving needs of patients, contributing to the local healthcare delivery transformation initiatives across Teesside.”
To find out more about Value Partnerships, visit siemens-healthineers.co.uk/value-partnerships
1 The statement by Siemens Healthineers Consulting described herein is based on projected results that may be achieved in the customer’s unique setting subject to all recommendations being implemented. Since there is no ‘typical’ hospital and many variables exist (e.g. hospital size, case mix, level of IT adoption) there can be no guarantee that other customers will achieve the same results.
Lead image caption: (From left to right) Lee Charlton – Regional Sales Manager at Siemens Healthineers Great Britain and Ireland, Gail Griffiths – Diagnostic Services Lead at North Tees and Hartlepool NHS Foundation Trust, Kelly Smith – Head of Radiology at South Tees Hospitals NHS Foundation Trust, Neil Lincoln – Head of Imaging Sales at Siemens Healthineers Great Britain and Ireland, with the new SOMATOM X.Cite CT scanner from Siemens Healthineers.
This article was kindly supported by Siemens Healthineers.