Insource chosen as trusted data partner for NHSE reporting by Tower Hamlets GP Care Group

Tower Hamlets announces Insource as managed services partner for automated data acquisition from EMIS and CSDS commissioner reporting.
Insource Ltd, a leading data management provider to the NHS, has been chosen by Tower Hamlets GP Care Group as its trusted data management partner. The first stage of the engagement will be to take data from the EMIS community system covering the 33 GP practices throughout the borough of Tower Hamlets, standardise it into a fully validated, single source of truth and automate the submission of Community Services Data Sets (CSDS) to NHS England.
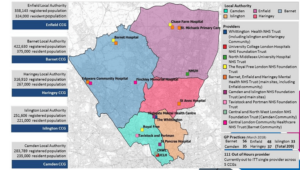
Tower Hamlets GP Care Group is an independent healthcare group that brings together 33 GP practices and seven primary care networks to better support the local Tower Hamlets population. As a GP Federation, the group provide a number of primary care and community health services including 0-19 years Health Visiting and School Health, Out of Hours GP services, and the Urgent Treatment Centre based in the Royal London Hospital.
With the recent mandate from NHS England that all community providers formally complete the CSDS submissions, the GP Care Group found they were spending inordinate amounts of time doing searches on EMIS on their KPI activity and downloading CSV files to do the monthly reports for their 0-19 services.
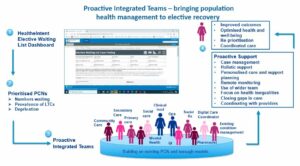
Zainab Airan, Chief Financial Officer at Tower Hamlets GP Care Group CIC, commented, “Whilst we originally brought Insource on board to extract the data from EMIS for our CSDS reporting, we rapidly realised the value of that core data for our own performance and business management.
“The data tables from EMIS are all over the place. Insource takes that data, makes it clean and usable, and automates our monthly NHSE reporting. But now we also have near real-time activity data for our own use. We can sit our own systems, such as Power BI, on top of this unified data to get quite sophisticated analyses.”
This single version of the truth will also be shared with frontline staff, such as health visitors, so they can track where they are with their contractual KPI targets and see how many 1-year checks are due this week, or how many new birth visits are outstanding. It will give everyone from the executives to the frontline the same data at their fingertips. So all have better insight into how they’re performing and how to make service improvements.
The GP Care Group also recently won a tender for 0-19 services in the nearby London Borough of Waltam Forest, whose GPs also use EMIS. They now aim to mirror what they are achieving in Tower Hamlets, within Waltham Forest and ultimately do dual CSDS submissions to the two NHS Commissioners.
Insource are providing the data management and reporting solution as a fully managed service on the Microsoft Azure cloud platform, initially across Tower Hamlets then, when needed, across Waltham Forest.
Zainab Airan concluded; “With over 500 staff, we are a medium sized independent care organisation, but chose not to maintain in-depth data management skills in-house. We prefer to leave the data management to the experts and to get on with our core business of clinical care. We are very excited about this project and Insource are doing a fantastic job. They truly are a trusted data partner that will allow us to scale as our business develops.”
Lee Bellis, Sales Director B2B Partnerships for Insource, stated: “The GP Care Group are innovative thinkers and have some exciting plans in the offing including expanding their services and potentially linking to children’s centres. But the big breakthrough here is being able to access proprietary EMIS data and making it usable, as an application-independent data source, for KPI tracking and internal performance management. This is big news for all GP and Community providers and is an obvious next step for Insource.
“We are seeing more and more of our customers taking up our managed services options. Our ground-breaking data management solutions and deep NHS knowledge, developed over 20 years, is proving very attractive to clients. Our multitude of NHS-tested data feeds is growing all the time and we can get even complex sites operational within weeks rather than months.”
About Insource
Insource leverages powerful data to help healthcare organisations drive better patient outcomes, streamline operational efficiency, and extract essential insight by ensuring all foundational data is accessible for informed decision making – despite the legacy infrastructure.
Their leading elective care solutions suite supports the patient pathway management, statutory reporting, and capacity planning challenges of the whole organisation. With over 20 years’ expertise, more than 55 acute, mental health and community trusts, health boards, ICSs and independent providers currently use our services. The Insource data management platform enables informed trust-wide management, ICS insight and control, and partner solutions innovation.
For more information contact info@insource.co.uk.
About Tower Hamlets GP Care Group CIC
Tower Hamlets GP Care Group is an independent healthcare group that was formed in late 2013 to enable General Practices in the area to be more involved in the local commissioning of health services. It brings together 33 GP practices and seven Primary Care networks to better support the local Tower Hamlets population and to work alongside other healthcare providers in the Borough. As a GP Federation, the group provide a number of primary care and community health services including 0-19 years Health Visiting and School Health, Out of Hours GP services, and the Urgent Treatment Centre based in Royal London Hospital.
Employing over 500 staff, Tower Hamlets GP Care Group also leads the provision of innovative, high-quality, responsive and accessible health care services in the area and is one of six organisations that form Tower Hamlets Together, the borough’s health partnership. This brings hospital, community health, mental health, adult and children’s social services, public health, and the voluntary sector together to provide comprehensive health and social care to the community. This ensures a more coordinated approach to providing services, reducing duplication and improving the overall experience and outcomes for the patients who need them.