Using integrated care to live healthier and happier lives

Angus Honeysett, Head of Market Access at Tunstall Healthcare, discusses putting citizens at the heart of care through technology, partnerships and integrated care to enable people to live happier, healthier lives.
The Government’s white paper, People at the Heart of Care, has a clear focus on integration and recognising the vital importance of improving quality of life and health outcomes. In particular, it promises £150 million of funding for several key areas, including assistive technology; improving the establishment and maintenance of digital records and data; upskilling the adult social care workforce in how to use technology; and bedding in wider digital infrastructure and cybersecurity within systems.
This is translated into the core objectives of integrated care systems (ICSs) as greater integration and more funding will enable them to facilitate the delivery of high-quality local services and citizen-focused outcomes.
The system will operate at three levels – integrated care partnerships, integrated care boards, and provider collaboratives – building better system-level knowledge of the needs of people so that they can receive more support closer to home, which includes some outpatient and diagnostic procedures.
People can stay independent for longer because health providers and community-based services will support those with the most complex needs outside of hospital settings. As the work of ICSs begins, now is a pivotal time that will shape our resources for decades to come.
Technology and cultural change
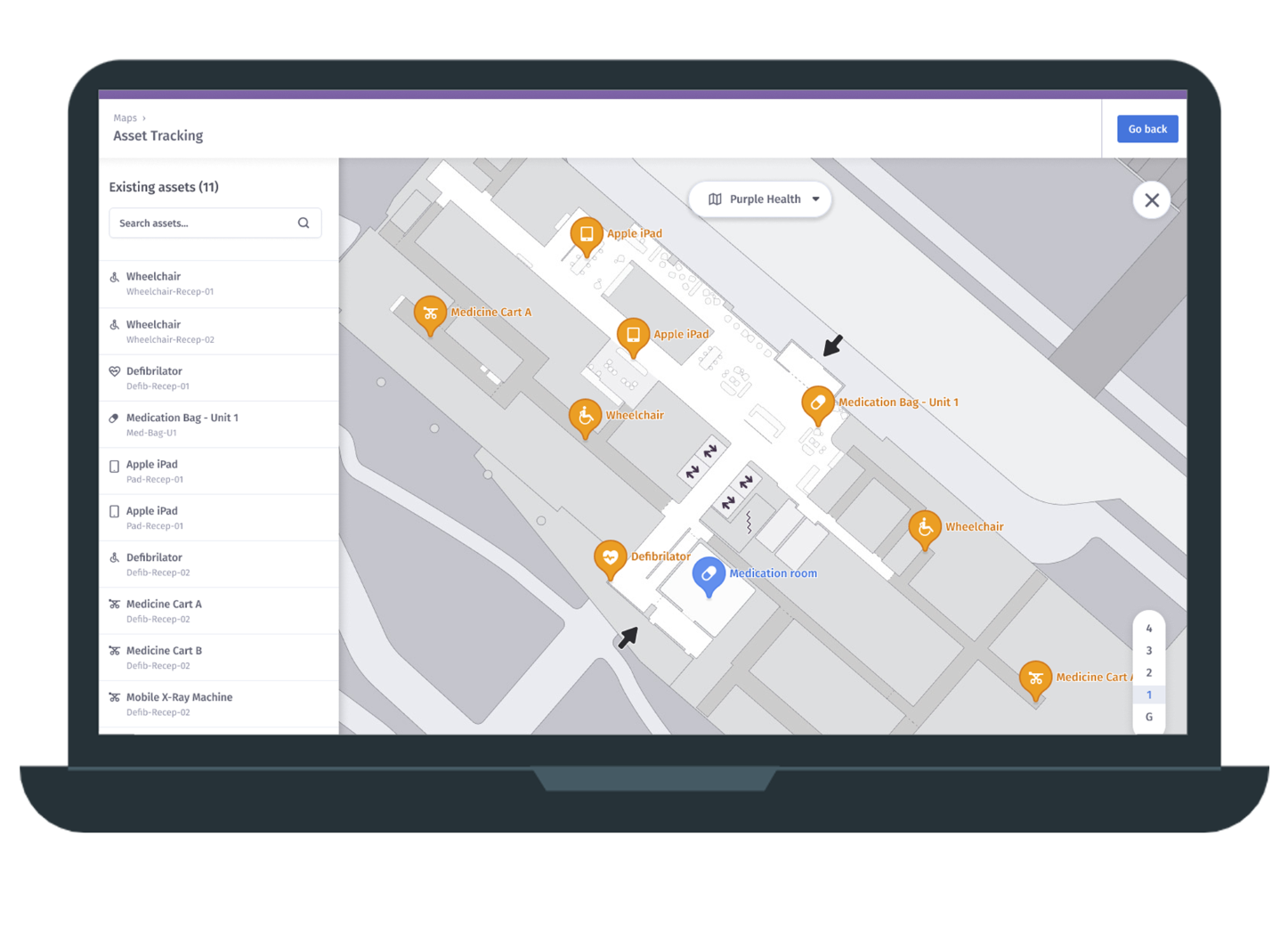
As ICSs continue to develop, the focus on driving digital systems that place citizens at the centre of service design and delivery will increase. Yet to deploy technology effectively, there are significant cultural challenges to overcome.
Technology has historically been seen as an addition to existing resources – a ‘nice-to-have’, rather than a means of transforming models of support. This has led to difficulties in integrating technology effectively. Cultural change is required which in turn needs early engagement.
Top-down leadership is needed to ensure stakeholders have input at an early stage into how technology can help them and the citizens they support. There are still workforce concerns that need to be addressed and stakeholders need to understand that technology is an enabler for better services, not a replacement for human contact.
Using technology to support people can be low-cost, thereby enabling more people to have digital solutions integrated into their care provision. This in turn gives professionals the ability to provide preventative care and engage with citizens so that they can stay at home for longer with an increased quality of life. Likewise, relatively low-cost telecare systems can help to avoid hospital admission and delay and prevent the need for residential care, and reduce carer burnout.
Understanding the barriers that we face and adapting as things change – not being driven by contracts, but by providing solutions – will ensure innovation continues to flourish. To successfully build solutions however, healthcare services must first understand the problems that are faced by people on a daily basis, with the recognition that this will change between individuals. The more we understand these problems, the easier it will be to co-design straightforward and effective strategies and solutions.
Technology is a quick win for ICSs and if used effectively, can free up the time for the workforce and other stakeholders, enabling them to become more productive in providing support to citizens that need it most.
The aim should be to embed technology so that outcomes are at the centre of all support that is provided, instead of endless form-filling, unnavigable processes and a bureaucracy which sees too many people get lost in the system, rather than receiving the support they need. It puts both power and opportunity in the hands of citizens and communities, providing solutions that are easy and efficient to access.
Collaboration and integration
Working together is in the interests of the public and all stakeholders, and greater integration, co-design and uptake of technology will enable an increase and improvement in the solutions that are available. This will also ensure that services can meet the population’s needs, saving taxpayers’ money through cost-avoidance to the system.
The formation of ICSs provides a unique opportunity to consider and pursue shared common goals. Health and social care must work together to have a positive and long-lasting impact on population health, to ensure citizens are at the heart of decisions about the support they need.
Our services are all intrinsically dependent upon each other which is reflected in the establishment of ICSs. If care delivery is ineffective, it places increased pressure on our health system, therefore leading to an inability to support citizens. Healthcare services need to have a truly joined up, integrated approach where they listen, understand everyday needs and work together to bridge gaps in resource allocation, including funding flow, which needs continued reform to drive system change.
When we deliver successful and integrated services, the benefits flow through the system from primary to secondary care, to community and social care. With the right approach, citizens can stay in the place of their choice for longer, delaying the requirement for more expensive and complex solutions.
Empowerment and control
The UK’s ageing population means there is little choice but to look at alternative ways to deliver support, in order to cope with increasing demand and more complex needs. The increased integration of technology and its use not only enhances the care that people receive, but also enables them to remain at home for longer, increasing the efficiency and capacity of our systems.
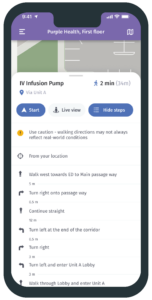
As we continue to invest and integrate technology into our services, it gives citizens greater ability to become more involved in how their health and wellbeing is managed. Data plays a particularly important role in empowering citizens to manage their own conditions as through technology such as telehealth, they can take their own readings and share these with the right people at the right time.
For citizens to be fully empowered, they must be engaged with and made a part of decision making around their care, and also understand the benefits that technology can bring, alongside how to use it.
Through the use of clear language, healthcare systems can communicate more effectively with citizens and build links between the technology that they already have and regularly use, and the technology that can support their health and wellbeing through new services. This in turn should reduce fear of the unknown and help drive a culture change at both local authority and citizen level.
By integrating services through ICSs and investing in the next generation of technology, it’s easier to engage families, friends, and communities in supporting early, proactive, and preventative interventions. Digital innovation presents opportunities to improve citizen experience, supporting better quality and greater reliability of service provision, providing enhanced solutions which are tailored to meet specific needs.
Looking to the future
ICSs and their development provide a timely opportunity to revolutionise our health systems and put citizens at the heart of care through the delivery of better outcomes and cost reductions. However, challenges remain, such as the UK’s move from analogue to digital communications networks.
This will require significant investment from the public sector at a time when budgets are already under extreme pressure, however, this brings a once in a generation opportunity to modernise, improve and shift thinking from a reactive, to a proactive delivery model. AI, machine learning and the use of data are hugely important to this.
Using data in a proactive and predictive way means issues can be highlighted early, which is in everyone’s best interest. The more that citizens are involved and engaged with data, including taking their own readings, the more they’ll understand how to more effectively manage their health and wellbeing on a daily basis.
By educating service professionals and the public on the value of data and how it can be used to transform health and care provision, people will become more comfortable with their data being used in a real-time setting.
With increased funding, improved decision making through ICSs, and better integration of technology, we will be able to drive reconfiguration and collaboration. It’s essential that service providers and citizens are involved in the digital transformation if we’re to innovate, embrace technology fully and successfully, and deliver new approaches which create benefits for both citizens and the system.
This article was kindly sponsored by Tunstall Healthcare.
For more information, please visit www.tunstall.co.uk.