Is the push for collaboration causing a retention crisis?
Rob McDonald, NHS Retention Services Manager at NHS Shared Business Services, asks whether exit interviews could hold the key to boosting NHS retention – a key goal of the NHS Long Term Workforce Plan.
Collaboration has been an NHS mantra for years now. According to all sources, no matter what the problem, collaboration (oh, and technology) will solve it.
But is that true? Intriguingly, my experience is that – far from being a panacea – the move towards collaboration might be exacerbating the NHS’s staffing problems.
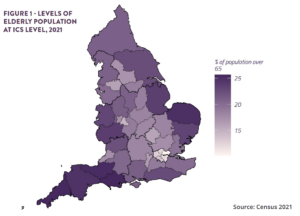
Don’t get me wrong. I’m a fan of collaboration. It helps to spread good practice. It reduces or eliminates inconsistencies. It enables organisations to pool their resources and benefit from economies of scale. So it’s perhaps not surprising that the entire NHS has been reorganised to encourage (or mandate) partnerships, exemplified by system-wide reorganisations like the establishment of ICSs two years ago.
The drive for productivity is resulting in mergers as services are scaled. The changes affect all organisations – from acute providers to community, mental health and learning disability services and Community Interest Companies. These TUPE transfers (Transfers of Undertakings (Protection of Employment), affecting many thousands of front-line staff every year, are frequently seen by senior managers as routine or benign. After all, the individual’s terms of employment are protected – so what is there to worry about?
The reality is that the changes are often poorly managed, can be unsettling and – I believe – are contributing so much to staff turnover that they’re having a significant impact on patient care.
What does it feel like if you’re one of those staff?
Thankfully, that’s a question we can answer. NHS Shared Business Services provides an exit interview service, which I am privileged to run. We’ve done more exit interviews in the past three years than most people do in a lifetime. I say that as a statement of fact, not a boast!
One of the questions we’ve started to ask leavers is whether uncertainty around, or the impact of, mergers has influenced their decision.
The answer is yes. We’re finding that nurses in particular often cite service mergers as contributing to their desire to leave, frequently in combination with other factors, such as general stresses of the job.
It goes without saying that this is a problem. The NHS’s long-term workforce plan highlights the need for up to 190,000 additional nurses by 2037, requiring retention rates to improve by around 15 per cent over the course of the plan. Losing nurses has knock-on effects way beyond the immediate impact on patient care. The cost of recruitment to backfill; the cost and time of additional training; the stress on team members who have to provide cover and the cost of overtime – all of these erode both money and goodwill.
The recently published NHS staff survey confirms this. Although most of the People Promise indicators showed a modest improvement, many of the numbers are still concerning. Some 30 per cent of respondents said that they felt burnt out by their work, and 34 per cent found it emotionally exhausting, yet only around half said they felt able to make improvements happen or be involved in change.
The good news is that this can be fixed. Mergers and reorganisations do not need to make staff feel disempowered and uncertain. In fact, when handled well, they can have the opposite effect.
To do this takes time, care, and skill – I’ve provided a few hints below, based on the feedback we’ve been getting.
Uncertainty about a merger is often more damaging than the merger itself, so communication really is key. People subconsciously “triangulate” information – that is, they won’t absorb or believe it until they’ve heard it from three different sources. So think about what level of communication you might need, then triple it.
Identify flight risks. This is something we’ve done for years at NHS SBS; we even have an algorithm that predicts people at risk of leaving. Then take proactive action to address their concerns and bring them further into the fold. Leavers often tell us their manager knew they were thinking of leaving; managers, by contrast, tell us the resignation came as a surprise.
Conduct exit interviews – and use the data you collect. I may be biased, but I think exit interviews are possibly the most important conversation you can ever have – more important even than recruitment interviews. Yet, remarkably, the standard approach is for an automated tick box survey to be sent to leavers upon resignation. The response rate is usually around 30 per cent and the greatest reason for leaving is ‘unknown’ – in other words, the path of least resistance to complete the survey without discussing any real issues.
Finally, remember – a resignation doesn’t have to result in a leaver. Is there a feeling that once resignation is given, the horse has already bolted? I think there is. Yet when I ask leavers whether they would have stayed if somebody had done something differently, the answer is often yes.
Resignations can be withdrawn. And sometimes, a conversation is all it takes to retain a valued and valuable member of staff.
Given that the magic roundabout of change in the NHS is unlikely to slow down any time soon, learning to support and empower staff through periods of uncertainty is critical.
I’d love to hear from readers about their experiences of change – particularly the impact of service mergers on retention and how you use exit interviews. Contact me at Rob.McDonald1@nhs.net.