Vic Townshend: ‘Whole person’ understanding is reliant on intelligence-informed decisions

Vic Townshend, Programme Director for Population Health Management (PHM) at Lincolnshire ICS, speaks with Public Policy Projects’ Ameneh Saatchi.
Building capacity and capability for population health management (PHM) is perhaps one of the single most significant enablers of truly integrated care and ambitions for England’s 42 integrated care systems (ICSs). But while every ICS will place significant priority on establishing comprehensive PHM, immediate service pressures and restricted resources have led to mixed results across the country.
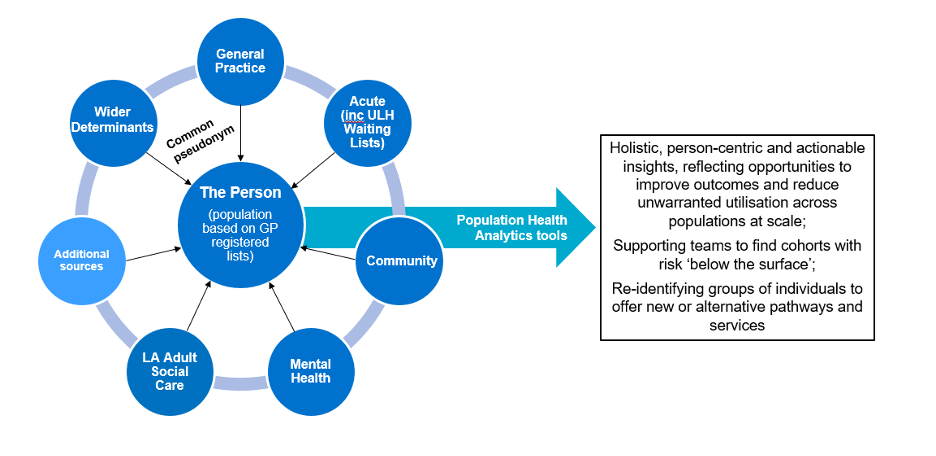
In Lincolnshire, the ICS has established the Lincolnshire ICS Population Health Management Programme, which uses a ground-breaking person-level linked dataset, recognised as one of the most extensive in the country. The Lincolnshire Joined Intelligence Dataset covers 100 per cent of the local GP registered population. It encompasses a range of data sources, including primary and secondary care, adult social care, elective waiting lists, deprivation indices, social vulnerability and isolation measures from the Office for National Statistics, Census data, and community asset registers.
This initiative originated with the NHS England sponsored Population Health Management development programme, which allowed for the system to test what PHM offered and supported the first linked dataset to be created for a proportion of the county’s population. Other systems do have linked datasets, but there are none currently known that have the same extent of sources and population coverage.
“I worked closely with the Director of Intelligence and Analytics [Katy Hardwick],” says Vic, explaining that the team entered a partnership with Optum UK, to build the first ever linked data set in 2019, which initially covered about 30 per cent of the population. “This gave us data joined at the personal level, allowing us to see a person’s journey through health and ill-health and how they interacted with services across Lincolnshire to support their needs.”
The data science tool employed by Lincolnshire ICS focuses primarily on measuring health and care utilisation across different contexts, emphasising unit of activity and associated indicative costs. Traditional metrics, such as length of stay are incorporated, offering a comprehensive view of resource utilisation. Moreover, the tool’s versatility allows for customised presentations of intelligence, enabling users to tailor insights to their specific needs. Insights into health inequalities are facilitated by comparing cohorts of individuals, shedding light on variation in outcomes and contributing to high quality decision-making.
In addition to traditional metrics and the sources listed above, the Lincolnshire dataset also encompasses prescribing and medicines utilisation data, facilitating a holistic, system-wide understanding of health and care activities, service utilisation and outcomes. The dataset captures activity from all community, acute and mental health services, drawing from data recorded in trusts’ National Minimum Data Sets. This ensures seamless integration of data, irrespective of where individuals receive treatment – even if that treatment is outside of Lincolnshire ICS.
In healthcare, intelligence-informed decision-making stands as a crucial factor in navigating complex systems effectively. Vic emphasises the importance of this approach, highlighting how linked data allows for a comprehensive understanding of the impact of interventions across healthcare settings.
“The linked data set allows us to identify where opportunities are for intervention and change [and] where we’re doing well,” Vic explains. “What it doesn’t tell us is what we should do with it, but it starts to prompt leaders to ask the right questions… there’s nobody in our system that just has diabetes, which brings into question why we are providing services for diabetics in silo when they have more than one long-term condition and are subject to many other wider determinants of health, such as deprivation.”
This enhanced visibility helps stakeholders to identify both direct and indirect benefits and drawbacks of interventions, leading to better-informed decisions.
“The linked data set allows intelligence-informed decision-making, [meaning] we can now see the impact of our actions across our organisational borders and identify indirect benefits and disbenefits. So, we can track how changes in general practice are improving outcomes across other services, or vice versa.”
The inclusion of indicative costing within the linked data set also provides insights into resource allocation and workforce interactions. This allows for a more subtle understanding of how resources are utilised within the healthcare system, facilitating efficient resource management and optimisation.
Evaluation plays a pivotal role in assessing the effectiveness of interventions and changes in healthcare delivery. Vic underscores the necessity of robust evaluation, encompassing both qualitative and quantitative measures. However, Vic also acknowledges the challenge of maintaining the usability of the linked dataset while incorporating qualitative elements, emphasising the need for flexibility in its development and usage.
“Intelligence-informed decision-making becomes your North Star; you’re all following the same intelligence that steers in the same direction, wherever you work within the system. It has allowed us to robustly evaluate qualitative and quantitative outcomes, so it’s not just about what we can measure in the dataset, but working with personalisation, understanding what outcomes are important to people.”
Overall, the linked data set serves as a valuable tool for identifying opportunities for intervention and making informed decisions that lead to improved outcomes for patient and wider health system.
Vic’s journey into PHM stems from a diverse background, transitioning from the RAF as a meteorology officer, to a decade in general management in healthcare, to change management in complex systems. A keen interest in data analysis has been the nexus between various positions throughout her career.
More recently, Vic has begun addressing performance improvement challenges in healthcare, focusing on the interconnectedness of prescribing practices and care pathways. As Director of the Population Health Management programme in Lincolnshire ICS, she emphasises the need for comprehensive, intelligence-informed decision-making in healthcare leadership, seeing it as pivotal for driving systemic change and improving outcomes. For Vic, PHM represents a transformative tool with the potential to fundamentally change healthcare systems and improve outcomes for all.
The inequality challenge
Intelligence Leads and Chief Analysts working within ICSs will have increasingly important roles in navigating the complexities of health inequalities. Such roles require skill sets that can play a crucial role in generating intelligence to inform various inquiries regarding clinical care outcomes, health and wellbeing, and wider determinants of health. By fostering relationships with them, healthcare professionals can gain access to previously untapped data sets or intelligence that can address longstanding questions or concerns.
While population health itself is not a new concept, the current level of focus being placed on PHM requires significant new infrastructure support, the need for which may not yet be universally recognised within individual health systems. Therefore, she advises initiating discussions with intelligence teams to explore existing available data and infrastructure.
Vic stresses the importance of incorporating intelligence specialists or analysts into discussions alongside clinicians and decision-makers. This tripartite arrangement ensures that data-driven insights inform decision-making processes effectively, leading to more informed and impactful strategy.
Wound care from the lens of population health management
Vic underscores several key priorities essential for improving Wound Care outcomes:
Consistent documentation on electronic systems
Vic emphasises the importance of developing consistent documentation of wound care activities on electronic systems across frontline services and at strategic level. This consistency ensures accurate data collection that is crucial, not only for clinical records, but also for evidence-based decision-making and outcome evaluation. This is something Lincolnshire ICS will be working to develop further, as Vic identifies a challenge in ensuring consistency across local teams to capture all necessary data for wound care. Addressing this challenge is fundamental for systems to improve efficiency and workforce challenges in the community but may require additional resources and strategies to improve documentation practices.
Personalised care approach
Vic discusses the need to personalise wound care, highlighting that different individuals may require different approaches based on their specific needs and preferences for self-care. This personalised approach ensures that care is tailored to everyone’s circumstances, improving overall outcomes.
Training and applying best practices
Ensuring that clinical teams involved in wound care across various organisations are trained in, and consistently utilise, best practices. This helps standardise care delivery with the aim of adhering to established standards and protocols and improves overall quality of care.
Evaluation and continuous improvement
Establishing mechanisms for evaluating the effectiveness of changes made in wound care practices and processes. This iterative approach to improvement allows for ongoing refinement and optimisation of care delivery. This involves identifying what works, what doesn’t, and adjusting accordingly to continuously improve care delivery.
Communication and engagement
Vic underscores the necessity of effective communication and engagement strategies to drive change and improve outcomes for individuals. Engaging the workforce and the population is essential for raising awareness about available treatments and promoting better understanding of wound care options.
Extending pharmacy services – the pros and cons
Vic acknowledges the potential of community pharmacists in wound care as they are in the heart of communities, close to the patients, and can have a further role in early intervention. But she raises concerns about the sustainability and consistency of extending their roles. Vic highlights challenges such as increased workload, inconsistent sign-up to extended services, and competing priorities within the pharmacy profession.
Vic also provides recommendations to apply population health management techniques to diabetes care for comprehensive support
Vic asserts the need to shift away from treating diabetes as a standalone condition and to instead adopt a holistic approach that addresses individuals’ overall health needs. She advocates for integrated care models that offer comprehensive support, ensuring that individuals receive assistance beyond diabetes management alone. This approach aims to improve overall health outcomes and reduce the likelihood of complications associated with diabetes, such as leg ulcers and amputations.
Empowering prevention strategies
Furthermore, Vic highlights the importance of prevention strategies in combating diabetes. She stresses the need for a cohesive and proactive focus on prevention, encompassing primary, secondary, and tertiary prevention efforts. By investing in preventive measures and proactive interventions, such as health and wellbeing initiatives and collaborations with voluntary sectors, individuals can be empowered to manage their diabetes effectively and avoid frequent visits to healthcare providers.
Personalised care: addressing individual needs
Lastly, Vic underscores the significance of a personalised approach to diabetes care. She advocates for a strengths-based conversation that empowers individuals to take charge of their health while ensuring that healthcare systems meet their personal needs. By tailoring care plans to individual circumstances and preferences, healthcare providers can address inequalities and deliver more effective and meaningful support. This collaborative approach involves engaging individuals in decision-making processes and considering factors such as housing, employment, and social support to create sustainable and equitable healthcare services. Figure 1 below demonstrates how population health analytics tools can improve outcomes and efficiency.
Conclusion
Vic emphasises the critical need for consistent documentation of wound care activities across all levels of healthcare delivery. This ensures accurate data collection, essential for evidence-based decision-making and evaluating outcomes. Additionally, she underscores the importance of a personalised care approach, recognising that individual needs may vary significantly. Training in best practices, continuous evaluation, and effective communication and engagement strategies are identified as key priorities to drive improvements in wound care delivery.
However, a significant challenge arises from the inconsistent capture of data by community nurses. This gap in documentation poses a barrier to comprehensive data analysis and evidence-based decision-making. Addressing this challenge will require focused efforts to improve documentation practices and ensure that all relevant data are captured accurately. By prioritising efforts to enhance data collection consistency, healthcare providers can strengthen the foundation for effective wound care delivery and evaluation.
What’s next?
Diabetes and wound care are the second and third highest expense to the health system respectively, and impact millions of people in the United Kingdom. Public Policy Projects is launching the second part of its Diabetes Care programme in the autumn of 2024 called ‘Holistic approaches to diabetes care – treating the whole patient’. Vic Townshend will be presenting on 2nd December, in London at the PPP Wound Care conference.
Contact Ameneh Saatchi, Director of Market Access for Diabetes and Wound Care, should you wish to learn more about these programmes: ameneh.saatchi@publicpolicyprojects.com