Taking practical steps to address a growing crisis in domiciliary care

John Bryant, Head of Strategy and Development for Torbay Council, outlines a series of practical steps to enhance the role of the care worker and address the growing crisis in domiciliary care.
The solution to the domiciliary care crisis is to enable the sector to do more, not to simply ask more of it. The distinction is important, as the development of integrated care provides opportunities to enhance system efficiency like never before. And yet, the scope of what could be asked of, and performed by, trained, supported, committed community-based practitioners is yet to be fully explored or achieved.
All the while, the expectations of those receiving care, and certainly those considering a future career in health and care, are greater than they have ever been.
To meet these ever-rising expectations, system leaders are likely to find fertile ground in looking to better embrace the assets that already exist within the system. This includes domiciliary care workers, whose skillset could be expanded and developed, a move that could encourage others into the system. This can happen by re-positioning the expectation, skills and rewards to produce and provide, for example, enhanced wellbeing services (EWS) provided by enhanced wellbeing practitioners (EWP), of which domiciliary care is a major component among a portfolio of beneficial interventions and service provision.
The 6Cs of care are prevalent within our frontline domiciliary partner staff; the opportunity is there to optimise their engagement and knowledge of patients and clients to:
- Support retention and recruitment
- Respond to the discharge and reablement challenges
- Drive early intervention and prevention
- Offer a developed interface with general practice
- Engage with population health management
The support of these four key drivers for public service change: politics, policy, measurement and money, are positioning us as never before to achieve success. The government’s social care reform white paper, People at the Heart of Care, connects to the £5.4 billion pledged for adult social care reform between 2022 to 2025. It is notable that healthcare is a major beneficiary of this funding in early years, however within the policy of integrated care the opportunity exists to bring about radical, beneficial system reform from the outset.
“Together, these measures aim to put people at the heart of social care and move us towards our 10-year reform vision.”
(Department of Health and Social Care, 2022).
These themes were also present in the subsequent integration white paper, Joining up Care for People, Places and Populations. The measures set out in the paper provide clear areas of opportunity, focus and policy support.
A growing crisis
These government white papers are in no small part a response to a care crisis the likes of which we have never seen. One key element of that is domiciliary care, the unseen service that is delivered behind the front doors of our communities to keep people safe, comfortable, medicated and cared-for. For over a decade the policy has been to bring care closer to home, and the People at the Heart of Care paper reinforces that. The Covid-19 pandemic has compounded the need to ensure people are cared for and supported in this way, minimising their movement between different health settings to reduce infection risk.
“The endeavours of care providers to recruit at this level should be celebrated alonside any other part of the system that has been able to do the same”
Present estimates indicate that there is a care shortage/vacancy rate of 17 per cent which equates to at least 100,000 jobs based on Skills for Care data in England. Given the challenges in recruitment felt by providers, there can often be a projection that care providers are not ’good‘ at recruitment. However, in looking behind the headlines we find that in one area, Torbay, care providers have increased their capacity through recruitment by 39 per cent in the 18 months leading to September 2021. The problem is that the demand for their services has totally outstripped this staffing influx, increasing by 47 per cent in the same time period. This trend is consistent across the country’s health and care ecosystem.
The endeavours of care providers to recruit at this level should be celebrated alongside any other part of the system that has been able to do the same. If organisations who have been able to recruit as well as Torbay have done are finding it difficult, is it probable that any other part of the system will do better?
The Health Foundation recently published research suggesting that over a million more health and care staff will be needed in the next decade to meet growing demand for care. What is clear is that these shortages were well established trends before the Covid-19 pandemic. If the challenge of capacity is to be permanently addressed, then retention followed by recruitment is essential – as any marketing of roles from ‘the system’ will be trumped by the messages communicated by those working in or leaving the services.
Recognising a new future, communicating that and providing examples of what could be achieved will produce opportunities for beneficial results.
Practical steps
In this respect, returning to the domiciliary care issue, what might emerge if we were to turn the issue on its head?
To address the crisis currently seen in domiciliary care, I propose a series of practical steps to enhance the role of the care worker and to use the ICS framework to transform system level efficiency:
- Addressing the domiciliary care shortage: expand the potential of the service and provide those delivering it with more responsibility and control by becoming EWPs
- Supporting the community nursing challenge: offer them the opportunity to have a wider team of EWPs at their disposal; enable them to work to the top of their licence
- To address GP availability: create neighbourhood teams of EWPs that are able to be with patients, directly support with digital literacy and connectivity, and be a physical presence to further enhance the experience of the remote general practice
- To reduce A&E admissions and improve the discharge process: use EWS to support the safe discharge of increasingly complex patients to optimise recuperation in at-home settings, have the digital skills and tools to monitor and report e.g. RESTORE2 for early intervention and re-admission avoidance, and be able to support reablement; the stepping stone to independence
- Develop greener care:reducing mileage by minimising cross-overs between staff and building a wider multi-disciplinary team
The practical possibilities for this are supported by the further development of the Allied Health Professionals strategy. The publication of the Allied Health Professions’ Support Worker Competency, Education and Career Development Framework received support from Trades Unions, Professional Bodies and Trade Union partners. Whether it is development within roles or providing new career paths, new forms of offer and opportunities are going to be central in encouraging a post-Brexit, domestic workforce into the social care and health sector; along with producing the impact value of those roles and associated care interventions which enable commensurate levels of pay and reward.
Underpinning all endeavours and quality care and support are the 6Cs of Care. These emerged as part of ‘Compassion in Practice’ and were rolled out by NHS England to all staff in 2014 with subsequent promotion to the wider care sector by the national body Skills for Care.
“But what cannot happen is that domiciliary care continues to be overprescribed without receiving more support or being allowed to expand its offering”
The characteristics of commitment, care, compassion, competence, communication and courage are prevalent throughout our community care partners and their staff. With that commonality between the professions what might we do to deliver even more fulfilling roles: more people doing fulfilling roles, more fulfilment within the roles, more roles in addition to the present ones that are also fulfilling?

This article seeks only to look at one small area of that; however, it is a vital area, being felt by the 957,000 people in the UK that receive domiciliary care and their families, along with the 822,000 staff looking after them (as recorded by RCN surveys). This, quite rightly, is now receiving both political support and national media attention.
The pandemic should be recognised as a catalyst for accelerated change, avoiding any sense of ‘once we’re through this we can get down to business as usual’. What has been done, and is being done in response to the pandemic, has demonstrated the creativity and pace of change possible as system partners have collaborated. Fostering and building on that is in itself both an opportunity and a challenge.
Across the sector there are understandable concerns of implementing radical service reform on an already exhausted and beleaguered workforce. But there are examples we can look to where workforce wellbeing is protected while simultaneously enhancing capacity and quality of care that motivates staff.
Some facts from one system
To service 800 clients in a 75-mile geographical perimeter, home care staff drive almost one million miles per annum. In work supported by the Health Foundation, it was found that at a (sub)urban travel speed averaging 20 mph, over 43,500 hours were being spent in vehicles; a substantial proportion of that could be put to new ways of working.
Work has shown that by reorganising the rounds, 5,220 hours of care could be released from the existing workforce. This would provide opportunities not only for more care to be delivered but importantly, and in respect of future retention and recruitment across the system, time for wellbeing, supervision, learning and development, accreditation of skills and assurance in their application. And with no extra hours of care being purchased.
In terms of application and the development of broader multi-disciplinary teams within ICSs, it was established that of the community nursing patients nearly 20 per cent were also social care clients. People were being visited by multiple staff in one day, requiring travel from multiple staff.
There are of course many activities and health interventions which can only be done by those with nursing and clinical qualifications. However, in approaching this issue with a mindset of curiosity, courage and compassion there are many interventions that could be performed in different ways.
For instance, one of the many activities that domiciliary care staff undertake is washing and creaming clients’ legs when there are wounds to be attended to. Nursing staff will then arrive to apply a bandage. While certain grades of wound clearly need nursing attention there are many at lower levels of severity that are capable of being attended to by a well-trained EWP – and of being checked on regularly, though less frequently, by the stretched community nursing complement.
Benefits of EWS for participants and for system development
Enhanced wellbeing practitioners:
- Feel respected and able to develop their domiciliary care roles, feel even more a part of the system and that their contribution is valued. This could lead to enhanced profile and esteem. The additional activity means more time with the client and the opportunity to further enhance the relationship that exists
- Opportunities will be presented to work in strengths-based ways and with programmes such as Making Every Contact Count, leading to enhanced wellbeing of the clients and a development of their connectivity and circle of support
- This leads to improved job/role satisfaction – improved retention leading to increased recruitment. Developed circle of support for clients, enabling them to step up towards independence and reduce their reliance on statutory interventions. Release of capacity for those with assessed needs to have their needs met and begin their journey towards well-being
Community nurses
- Feel an increased level of support with a bigger, more integrated, team available to them. They are then able to work with the more complex cases and make the very best use of their skills and knowledge while enabling and supporting other integrated team members to develop
- Through enabling better management of case-loads, job satisfaction is increased and stress is reduced. As the RCN has established, with 75 per cent of community nurses reporting that they had left necessary activities undone, the professional dissonance of the role is alleviated, supporting staff wellbeing and retention
- With the nursing and Allied Health Professional colleagues active in this way, early intervention and reductions in exacerbations of conditions lead to reduced admissions. With greater capacity, along with the skills to manage more complex discharges, hospital flow is improved
Benefits of EWS for health providers
Admissions through A&E:
- Are reduced by earlier interventions and the ability to deploy the highly skilled staff in the community to support patients and reduce the deterioration in their condition
- Improved flow through A&E with reduced admissions, enhancing the wellbeing of staff as well as the patients, and contributing to the enhanced application of funding to meet elective care
Discharges and re-admission rates:
- Are further improved with the skills and capacity made available to support increasing numbers of and increasingly complex patients. With the integrated approach to working and early intervention opportunities, people are supported to remain at home, with their condition even better managed and do not require a re-admission to hospital
- Skills and capacity across the community integrated team are available to support timely, safe discharge from hospital and discharge to assess and ensure people remain at home
- The patient/client gets less ill and recovers more quickly being supported by a team that has the resources, capacity and skills to meet their needs. This increases the ability for them to remain well or recover quickly in their home setting, which include care homes and supported living
- Increased numbers of people cared for closer to home with reduced exacerbations in conditions. Complex clinical requirements being met in community settings with both care-giver and the patient having a well developed strengths-based relationship throughout the care and support period, enabling a step up to independence
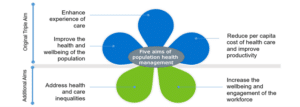
It is understandable that there will be anxieties associated with the shift in activities. In order to ascertain who delivers what and where to achieve the five aims of population health management (as illustrated below), the mantra to hold onto is right person, right care, right place, right time. Risk-managed prototyping using good design methodologies is key and implicit within the title on the tin of sustainability and transformation partnerships (the predecessor to ICSs).
There are many practical examples already available and still plenty of headroom for further development, which will accelerate the transformation in health and care models which are both sought for and needed.
Covid has shown us how much can be done in a short space of time; even with all the pressures in the system, GPs, acute trusts, AHSN and domiciliary care providers worked together to train 148 staff in the RESTORE2 methodology in just three months, with some going further to be trainers themselves.
Practical steps to developing and implementing enhanced wellbeing services
- Train domiciliary care and care home staff to use the protocols and develop relationships with primary care practices
- Ensure that training is accessible and that the nursing staff are corporately supported in the delegation of tasks
- Look to see if care packages are allocated by geographically focussed provider or on first-come-first-served basis, and what the mileage component to the care rounds is for providers
- Review the wounds being attended to in community settings and what best practice can offer in tackling the £5 billion cost of wound management
- Consult on ways in which the Allied Health Professions’ Support Worker Competency, Education, and Career Development Framework can be optimised
- Get the best facilitators and design thinkers, often found outside the system, to help ask the questions, listen and gather the answers and develop action-orientated plans with system partners – which includes the care unit, the patient/client and those caring for them
Whichever of the four policy drivers (politics, policy, money or measurements) one wishes to consider, they are captured within the Five Aims of Population Health Management; moving to EWS and development of the practitioners supports their delivery. Beyond this the one element that is maybe more implicit within the ‘petals’ below is capacity. EWS supports this explicitly.
Achieving more with less
In summary, below is the 30-second elevator review of how we can achieve more with less on the topic of domiciliary care.
More:
- Time to care, more time to be more caring
- Development and enrichment of roles
- Person-centred care
- Satisfaction with the role
- Retention
- Recruitment
- Prevention and early intervention
Less:
- Dissonance in the role and 6Cs
- Siloed working
- Variation in care team and discontinuity of care
- Dissatisfaction with roles and system design
- Turnover and leaving before retirement, or at the earliest opportunity
- Vacancy and cost to trying to encourage people into services
- Illness and cost
Addressing the care crisis
With the job-seeking public indicating that insufficient numbers of them wish to work in domiciliary care, now would be the time, supported by the policy of integrated care, to develop a new offer that enables truly integrated roles. This should seek to provide enhanced wellbeing services through an increasingly broad, multi-disciplinary, person-centred team.
To address this multifaceted care crisis, we should do more than seeking to invite people into traditional domiciliary care. The system might benefit from offering people a new role(s) that encompasses the domiciliary care that they are proud to already be doing, but also one that offers development, inclusion, satisfaction, esteem and commensurate compensation. This could become increasingly available if and when ICSs fulfil the potential that exists; one that reflects those stated aims within the recent white paper(s) and meets the five tenets of Population Health Management.
This should also note the observations of the CQC and their likely support to engage in discovery sessions for regulation alignment towards new ways of working. In doing so this should create a virtuous cycle towards a sustainable system, both financially and with capacity, through the delivery of integrated care.
John Bryant is Head of Strategy and Development for Torbay Council and an ICJ contributor. To contact John, become an ICJ contributor or to obtain a full reference list for this article, please write to news@integratedcarejournal.co.uk, and one of our Editors will assist.