NHS England releases its 2023/24 business plan

New plan focuses on cutting waiting lists, recovering core service performance, delivering on the NHS Long Term Plan and supporting digital transformation.
NHS England has released its business plan for 2023/24, setting out its priorities and commitments for the coming year. The plan identifies “three key tasks” for the NHS, namely; recovering core services and productivity; delivering the key ambitions of the NHS Long Term Plan; and continuing to transform the NHS for the future.
Also included are measures to support the NHS workforce through increased training, retention and modernisation of working practices, in line with the recently published NHS Long Term Workforce Plan, and to support the transition of staff to integrated care systems.
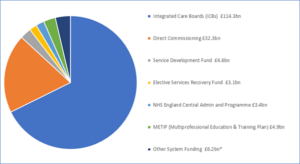
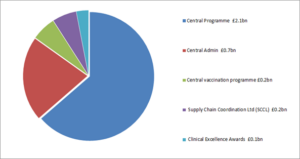
The document also includes a breakdown of the NHS’ commissioning budget for the year (see Figure 1), which stands at £168.8bn, up from £153bn in 2022/23, as well as that of the central admin and programme revenue funding (Figure 2). The majority of this fund – £114.3bn – will be allocated to integrated care boards (ICBs) to commission local services, while £32.3bn will be used to directly commission a range of primary care and public health services.
A further £4.9bn will be spent on workforce education and training via an annual investment planning process – the Multi-Professional Education and Training Investment Plan (METIP).
The full NHS business plan 2023/24 can be accessed here.
Below is a selection the NHS’s key commitments for the year 2023/24, as stated in the business plan, along with a some of the provisions included to deliver on these objectives:
Improving ambulance response and A&E waiting times
Increasing capacity: Dedicated funding for £1bn to pay for additional capacity, including 5,000 new beds; working with the ambulance service and wider systems to increase capacity supported by dedicated additional funding of £200m; the provision of £150m to build 150 new facilities to support mental health urgent and emergency care services.
Growing the workforce: The launch of a new targeted campaign to encourage retired clinicians, and those nearing retirement, to work in 111 rather than leaving the NHS altogether; making recruitment easier by reviewing the training and NHS Pathways licence requirements.
Reducing elective long waits and cancer backlogs, improving performance against the core diagnostic standards
Elective: Developing and implementing a new outpatient productivity programme that focuses on freeing up capacity; targeting improvement/transformation support to the most challenged providers, and clinical specialty pathways.
Cancer: The provision of more than £390m in cancer service development funding to cancer alliances to support delivery of early diagnosis and key operational priorities; a continuation of the rollout of non-specific symptoms pathways; supporting the rollout of targeted lung health check sites.
Diagnostics: Providing funding to support the development of pathology and imaging networks and the development and rollout of community diagnostic centres (CDCs) (£2.3bn of capital funding to 2025 has also been allocated to support diagnostic service transformation, including to implement CDCs, endoscopy, imaging equipment and digital diagnostics).
Improving access to primary care services, particularly general practice
Empowering patients: Transforming the NHS App to support the ambition for 75 per cent of all adults in England to be registered on the NHS App by March 2024; launching Pharmacy First (subject to a DHSC led consultation with Pharmaceutical Services Negotiating Committee) enabling pharmacists to supply prescription-only medicines to treat common health conditions where clinically appropriate.
Implementing modern general practice access: Supporting the transition to digital telephony; making high quality online consultation, messaging and booking tools available to general practice; investing in a new National Care Navigation Training Programme for up to 6,500 staff.
Improving maternity and neonatal services
Equity and personalised care: Piloting and evaluating new service models designed to reduce inequalities, including enhanced midwifery continuity of carer; acting on findings from the evaluation of independent senior advocate pilots as set out in the interim Ockenden report.
Retaining, growing and investing in the workforce: Funding a retention midwife in every maternity unit during 2023/24; strengthening neonatal clinical leadership with a national clinical director for neonatal and national neonatal nurse lead; working with the Royal College of Obstetricians and Gynaecologists to develop leadership role descriptors for obstetricians to support job planning, leadership and development.
Preventing ill health and narrowing health inequalities in access, outcomes, and experience
Major conditions and public health: Developing cardiac and pulmonary rehabilitation resources to support local decision making and improve access; delivering national services to support improvements in Type 2 diabetes prevention and remission services and national digital structured education support for Type 1 and Type 2 diabetes.
Screening and vaccinations: Developing and publishing a vaccination strategy and starting implementation in partnership with regional teams and ICSs; developing strategies for NHS screening and Child Health Information Services (CHIS).
Health inequalities: Publishing a healthcare inequalities strategy, with supporting resources including a new system accountability framework and framework for NHS action on inclusion health.
Building and developing the workforce for now and the future
Growing the workforce: Supporting expansion of the workforce and development of new roles aligned to key service development priorities; implementing the global health workforce strategy; delivering the 2023/24 METIP plan for medics, and clinical professions and develop the Clinical Placement Management System.
Culture: Co-producing management, talent and leadership development products, taking account of the Messenger review; developing and supporting implementation of interventions to deliver on the People Promise, improving staff experience and retention.
Digitisation
Ensuring that 90 per cent of trusts have an electronic patient record (EPR); developing and deploying a support offer to trusts undertaking EPR-related transformation and publish Minimum Digital Foundations guidance; providing practices with the digital tools to support Modern General Practice Access, and fund transition cover (for those that commit to adopt this approach before March 2025).
Developing the NHS App as the digital front door of the NHS; delivering new functionality for the NHS App, to help people take greater control over their health and their interactions with the NHS.
Procuring a Federated Data Platform, available to all ICSs, with nationally developed functionality including tools to help maximise capacity, reduce waiting lists, and coordinate care.
