Study of digital self-management service evidences a 50% reduction in A&E attendances for COPD patients
A study of a COPD digital supported self-management service delivered in Hull has achieved a 50 per cent reduction in A&E attendances and admissions for patients, resulting in significant savings for the local NHS Trust.
The study team were evaluating the Lenus Treat: COPD Supported Self-Management Service and have released early evaluation data, alongside an economic model, which indicate the service is both less costly and more effective than standard care.
COPD (chronic obstructive pulmonary disease) is a long-term progressive lung disease, which causes narrowing of the airways, making it difficult to breathe. It affects more than 1.7 million people across the UK, with almost 30,000 dying from it annually. Exacerbations caused by COPD are the second most common cause of emergency hospital admissions, accounting for 1 in 8 of all UK hospital admissions. The disease is predicted to cost the NHS £2.5 billion each year by 2030, largely because of the expense of these emergency admissions.
In Hull, emergency admissions for COPD patients over the age of 35 are nearly twice the national average, with 259.2 admissions per 100,000 compared to the national figure of 133.5 in the last available records during the pandemic. The city is one of the 20 most deprived districts/unitary authorities in England, with some neighbourhoods among the most deprived in the whole country according to the ONS.
However, researchers at Hull University Teaching Hospitals NHS Trust (HUTH), part of NHS Humber Health Partnership, have discovered early signs that offering patients Lenus Health’s digital support service, can reduce hospital admissions, with further potential to decrease the amount of time patients spend in hospital each year.
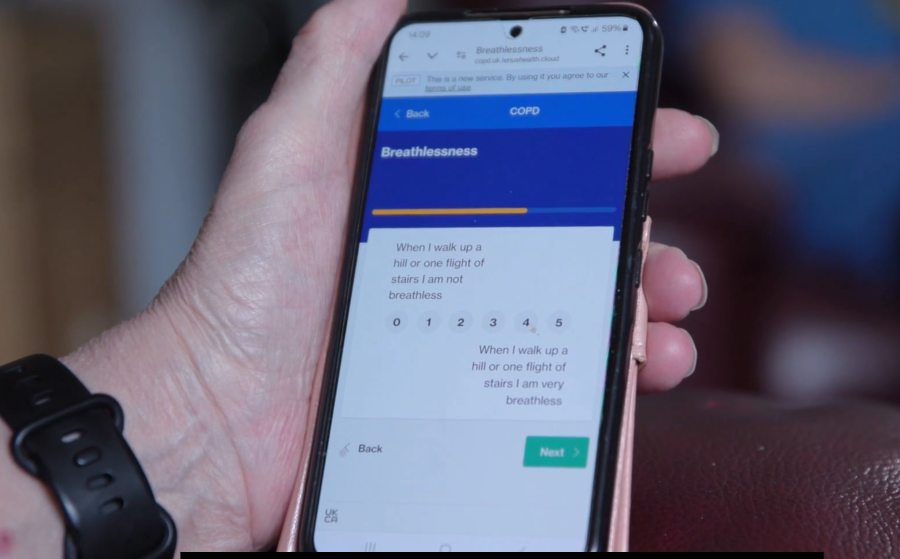
The Dynamic Rose study, funded by the Small Business Research Initiative (SBRI), recruited more than 100 patients from HUTH following an admission. Patients were then provided with a digital service to help them to recognise and self-report their symptoms, access self-management resources, and to directly communicate with the clinical team if there was cause for concern.
This potentially helped patients to identify when they were at early risk of exacerbation, so appropriate interventions could be actioned by clinicians, informed by the data captured from the patient, and shared in the service’s clinical dashboard.
Significant reduction in hospital admissions
In addition to the 50 per cent reduction in A&E attendance, interim results of the Dynamic Rose study also indicated a number of other impressive benefits as a result of the Lenus Treat: COPD Supported Self-Management Service. These included a reduction in hospital admissions of more than 50 per cent after the first month and a sustained reduction in hospital admissions of 45 per cent after three months compared to historic controls.
As part of an independent health economic evaluation undertaken by the York Health Economic Consortium funded through the project, the digital support service was modelled to be more effective and £1,749 less costly than standard care, per patient per annum.
By addressing the healthcare needs of COPD patients effectively, the digital support service from Lenus Health approach has been shown to improve patient outcomes but also reduce unscheduled healthcare resource use.
Paul McGinness, CEO of Lenus Health, said: “These results demonstrate that providing care teams with the right digital tools to virtually manage patients can improve health outcomes and release clinical capacity back into the system by reducing unscheduled hospital admissions. Our service was designed with patients and clinicians to align to their needs. It provides a supporting ‘digital hand on the shoulder’ of patients, while not being onerous for care workers to monitor and intervene when risk rises.”
Prof Michael Crooks, Respiratory Consultant at HUTH, said: “One of the characteristics of COPD is periods of worsening symptoms, called exacerbations. COPD exacerbations are a common reason for hospital attendance, admission and negatively affect sufferers’ quality of life. The Dynamic Rose study has provided early additional evidence, that builds on the work in Glasgow, that Lenus’s digital service can help to reduce the frequency of COPD exacerbations that require hospital treatment and admission. This has great potential to maintain patients’ wellbeing and also free-up valuable hospital resources.’’
Allyson, a 61 year-old patient using the service in Hull, said: “My confidence has increased since I’ve come under the team and on the app, it makes me more thoughtful, and I tend to not push it any more. Since I’ve learnt the breathing techniques, started filling out my daily questions, thinking about my condition, it has made a big difference. I’ve never gone so long without an antibiotic.”
The Lenus Health collaboration with HUTH follows a study with similarly impressive results of a 50 per cent reduction in hospital admissions and respiratory-related occupied bed days for participants at NHS Greater Glasgow and Clyde in Scotland. Full results and evidence from Hull will be published in clinical journals in due course.