A case study in effective integration: the Staten Island PPS

Collaboration, trust and community engagement will be central to successful long term reform of health and care. This is no different in the USA.
The pandemic provided many lessons, not least of which was that the health system could quickly pivot to less costly telehealth, digital and virtual care. For over two decades, these services were available but adopted reluctantly and not well capitalised upon.
One reason is that healthcare is faced with the inherent conflict between investment in bricks and mortar, and a model of care that is more patient-centred and community-based. The US model of care is heavily invested in expensive infrastructure and its healthcare bill is nearing $4 trillion, almost double the per capita cost of other industrialised nations. Despite this extraordinary expense, quality outcomes lag global norms, as does US life expectancy.
Delivery System Reform Incentive Payment programme
According to Forbes, US expenditure on healthcare is expected to be nearly $6 trillion by 2027. The redesign of healthcare is a matter of national importance, not just because of cost but the health disparities resulting from it. One strategy is the focus on moving from volume to value, as Michael Porter advocates in his book, Redefining Health Care.
The Delivery System Reform Incentive Payment (DSRIP) was designed to improve clinical quality while reducing costs and promoting the transition from volume to value. In April 2014, the Center for Medicaid/Medicare Services (CMS) approved New York State’s (NYS) Medicaid redesign waiver, known as DSRIP, in the amount of $8 billion over five years. To earn the maximum $8 billion valuation, performance on specific, pre-set quality and utilisation targets needed to be achieved with a focus on incentivising value. The waiver permits states to use Medicaid funding in ways not specifically authorised in Federal rules so that innovative strategies may be deployed to test new models of care using non-traditional services.
“Community engagement, trust and collaboration were keys to the success of the PPS programme.”
Joe Conte, Executive Director, Staten Island Performing Provider System
To achieve rapid change and capitalise on innovative strategies to affect nearly six million Medicaid recipients, NYS approved 25 provider networks, spread throughout the state. Known as performing provider systems (PPS), they were geographically disparate, with vastly differing population health needs and provider capacities. Their potential individual earnings over the five-year programme ranged from $45 million to $1.2 billion. Staten Island PPS (SI PPS) charted its own unique course improving population health outcomes while creating significant changes in the health care dynamic of the community.
Staten Island PPS background and programme description
Staten Island, with a population of about 500,000 is one of the five boroughs of NYC, with more than 30 per cent of the community covered by Medicaid. The SI PPS is a network of 70 medical, behavioural and social service providers, nursing homes, federally qualified health centres, primary care practices, and faith-based and community-based organisations. When the 1115 Waiver opportunity (which typically reflect priorities identified by the states and the federal Centers for Medicare and Medicaid Services) was presented to the community, great interest was demonstrated. The two major hospital systems were the anchor organisations.
According to New York State Department of Health, SI PPS funding was set at a valuation of roughly $208 million based on projects selected and clinical performance variables. Partner organisations attended facilitated workshops to analyse population health data to select 11 programmes (see table below) from among 50 offered. Over the course of a year, the process contributed to a sense of inclusion by the stakeholders and ownership of the implementation strategy devised for each of the programmes.
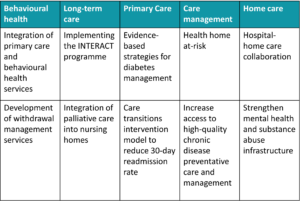
Table 1 illustrates the projects selected by SI PPS and the number of lives that needed to be “actively engaged” to achieve improvement goals. Each year, performance requirements and the number of lives increased and performance targets were reset based on prior year achievements. Certain indicators identified as critical to a programme’s success were associated with high-performance funds (HPF) that rewarded organisations for performance when a gap-to-goal of greater than 20 per cent was achieved. Depending on how many organisations achieved those metrics, the HPF could mean millions in additional revenue. In the Outcomes section, you will see that this resulted in a significant bonus payment to SI PPS.
System of care
To achieve performance goals, SI PPS used a standardised approach that focused on a system of care methodology. Systemic identification of gaps in services, skills, and community resources led to the design, implementation, evaluation, refinement, and sustainability of programmes. These addressed gaps identified from quantitative and qualitative assessments and have been implemented with SI PPS oversight, funding, and other resource support. Two use cases of the model are described below.
Major reorganisation of the community-based care model was at the core of DSRIP transformation, including the integration of medical providers in behavioural health clinics to provide physical health services to improve health outcomes and use of data to drive changes in the model. Staten Island PPS’ analytic platform showed that more than 50 per cent or preventable ER care was driven by five per cent of patients. The vast majority with behavioural health needs of non-emergent nature. Delivery of integrated behavioural health and primary care services to individuals diagnosed behavioural health issues ensures co-ordination of care for both types of services and reduced ER visits.
In nursing homes, SI PPS analytics demonstrated that sepsis hospitalisations were driving significant admission and re-admission rates. A quality initiative was created to focus on early identification and standardised treatment across all 10 skilled nursing facilities in Staten Island. Additional training, equipment standardisation and clinical protocols were developed. After 12 months, sepsis hospitalisations were reduced by 23 per cent and the gains continue.
The SI PPS programme relied on the use of business intelligence enabled by data exchange among partners, transforming traditional outcome strategies that produced excellent utilisation and population health improvement.
Technology platform: business intelligence
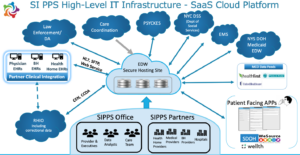
To create a data-driven culture and use business intelligence to guide programme design, innovative initiatives and performance measurement, SI PPS created an advanced population health management (PHM) ecosystem that monitors outcomes of care at an individual, practice and population level.
The PHM platform illustrated in Diagram 1 (below) integrated health data from multiple sources, including claims, clinical data, emergency management systems (911), law enforcement data, payor data and clinical event notifications (CEN) from the local health information exchange (HIE). The platform contained harmonised individual patient records and analytic tools to facilitate care delivery across Staten Island. The platform’s geo-mapping and hot-spotting capability made it possible to see geographic areas with service, health outcome and social determinant of health gaps. The tool enabled SI PPS and partner organisations to track progress toward outcome targets and provided a clear, comprehensive and population-based understanding of care quality and cost outcomes. SI PPS created its own social determinants of health system called WeSource to assess and refer clients to needed social services while linking to their clinical profile.
Highlights of PPS outcomes
2020, final performance metrics for the five-year programme were released. SI PPS was recognised as the top performer in NY and awarded $62 million in bonus payments.
Key outcomes of the programme include:
- A 400 per cent expansion of access to medication assisted treatment for people with opioid use disorder (Hospital Times, 2019)
- Reductions in ER use by more than 25 per cent for high-risk clients engaged in a comprehensive care co-ordination programme called HEALTHi, which provided critical time intervention to people with multiple complex conditions
- Avoidable hospital readmissions reduced by 25 per cent via intensive care co-ordination model
- Sepsis intervention programme reduced hospital transfers from nursing homes by 23 per cent and saved more than $3 million annually (Journal of Long-Term Care, LSE)
- Shelter to permanent housing program with NYC Department of Social Services (DSS) saved on average $25,000 per family
- Creation of training programme to educate and place certified recovery peer advocates (CRPA) and community health workers (CHW) in the ER and other high-impact settings
- Development of an asthma home visit programme for adolescent super utilisers
- Creation of SDOH network to assess and meet needs such as food insecurity, employment, training and housing for more than 28,000 families
- A safe prescriber programme educated prescribers about opioid alternatives and evidence-based prescribing algorithms reduced unnecessary prescriptions for opioids by 31 per cent
- Comprehensive cultural competency and health literacy training programmes for partner organisations delivered 70,000 hours of training to partner staff
Collaboration is key
Community engagement, trust and collaboration were the keys to success of the PPS programme. Although significant strides were made to begin to transform the delivery of care on Staten Island, much work is to be done locally and nationally to improve quality and reduce costs for the sickest and most vulnerable patients. Governments, payers and regulatory agencies must work rapidly to develop innovative payment systems that incentive value over volume, and to address significant health disparities among historically marginalised communities in an effort to reduce rising costs and poor health outcomes.
